As lawmakers debate major changes to the federal health law, it is important to understand what’s at stake in Connecticut. The Connecticut Health Foundation commissioned the Urban Institute to model the impact of the Affordable Care Act (ACA) on Connecticut, with a focus on state residents who might lack health care coverage without it.
“Our goal is for decisions to be made with good data and an understanding of the implications on people’s lives,” said Patricia Baker, president and CEO of the Connecticut Health Foundation. “We commissioned this analysis to document what is at stake as lawmakers consider significant changes to the health care system. We hope this measure of the current status of coverage in Connecticut provides a baseline on which to measure the impact of future reforms.”
The full report is forthcoming. Here are some of the key findings:
Connecticut’s uninsured rate would be almost twice as high without the ACA
- An estimated 198,000 Connecticut residents under 65 are uninsured this year, but without the health law, it would likely be 81% higher – 359,000.
- Put another way: For state residents under 65, the uninsured rate is 6.6%. Without the ACA, it would be 12%.
Minorities, people without a college education, and workers are disproportionately represented among residents who gained coverage under the ACA
According to the Urban Institute’s modeling, there are roughly 161,000 people who have coverage because of the ACA who would be uninsured without it. (Others covered by the health law’s Medicaid expansion or health insurance marketplace might have other sources of coverage if the ACA didn’t exist.)
Of the approximately 161,000 state residents who are covered because of the ACA:
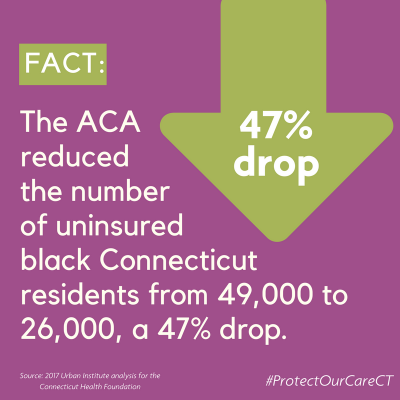
- 46% are people of color, including 23% who are Latino, and 14% who are African-American
- 40% are young adults ages 19-34
- 62% were not educated beyond high school
- 81% live in working families, including 68% in families with full-time workers
People with employer-sponsored insurance have new consumer protections because of the ACA
There are 1.9 million people in Connecticut with employer-sponsored insurance. Although most didn’t gain coverage because of the Affordable Care Act, aspects of their plans changed because of the health law. In particular:
- Their insurance now covers preventive services with no out-of-pocket costs to patients. This includes check-ups for infants, children and adults; cancer screenings; and contraception.
- Insurance plans cannot impose annual or lifetime coverage limits for essential health benefits. Before the ACA, insurance plans commonly set dollar limits on how much they would cover, leaving people who faced high medical costs – such as for cancer treatment or after a car accident – with significant financial burdens, often leading to bankruptcy.
People who don’t get coverage through their jobs have additional protections
Approximately 163,000 Connecticut residents buy coverage through the state’s individual market. Under the ACA:
- People cannot be denied coverage or charged more because they have a pre-existing condition. Before the ACA, many people with such conditions were unable to buy insurance. The Kaiser Family Foundation estimates that 522,000 Connecticut residents under 65 – 24% – have pre-existing conditions that could have left them unable to buy insurance before the ACA.
- Insurance plans sold on the individual market must cover 10 essential health benefits, including maternity care and mental health and substance abuse treatment. These services were often not covered by plans sold through the individual market before the ACA.
- Approximately 73,000 people receive federal financial assistance to lower their monthly premiums.

People with Medicare receive more coverage and lower costs for medication
Approximately 591,000 Connecticut residents are covered by Medicare. Because of the ACA:
- They now receive check-ups, cancer screenings, and other preventive services with no out-of-pocket costs.
- Those with annual prescription drug expenses between $3,700 and $4,950 – the “donut hole” – now receive Medicare payments to cover 60% of the cost of name-brand drugs and 49% of generics. Without the ACA, Medicare beneficiaries would receive no coverage for medication costs in this range.
The ACA cut uncompensated care provided by hospitals, doctors and other providers by more than 60%
- The Urban Institute’s projections indicate that in 2017, hospitals, physicians, and other health care providers would have delivered more than $1 billion in unreimbursed care to the uninsured without the ACA. Because of the coverage gains that occurred through the ACA, the amount of uncompensated care will be closer to $416 million – 61% less.
The ACA is responsible for more than $1 billion in additional federal funding for Connecticut
- In 2017, Connecticut is slated to receive $1.16 billion more in Medicaid funding and subsidies for private coverage from the federal government compared to what it would receive for Medicaid without the ACA.
- This additional funding has allowed Connecticut to spend $40 million less in state dollars on Medicaid than it would have without the ACA, while covering 138,000 more people through the program.
- Nearly 100 Connecticut organizations – including hospitals, nursing homes, community health centers, and state government – are receiving more than $62 million in federal funds made available through the ACA to help develop new models of delivering care intended to improve outcomes and slow the growth of health care costs.
Methodology
The Urban Institute’s projections compare actual coverage and costs in 2017 under the ACA to estimates of coverage and costs in 2017 without the ACA. The estimates are based on the Urban Institute’s Health Insurance Policy Simulation Model, which is based primarily on data from the U.S. Census Bureau’s American Community Survey.
A full report with additional data on the ACA’s impact on Connecticut overall and on specific groups is forthcoming.
For more information, please contact Arielle Levin Becker at 860-724-1580 x 16 or arielle@cthealth.org.